Gastric bypass surgery is a life-changing procedure that can offer significant weight loss and improved health outcomes for individuals struggling with obesity. However, the success of the surgery depends not only on the procedure itself but also on the dietary choices before and after the operation. The gastric bypass diet is carefully structured to support healing, minimize complications, and promote long-term weight loss. Let’s explore what to eat and drink before and after gastric bypass surgery to maximize its benefits.
Pre-Surgery Dietary Preparation
Before undergoing gastric bypass surgery, it’s essential to prepare your body for the procedure and optimize your nutritional status. Here are some dietary guidelines to follow in the weeks leading up to surgery:
High-Protein Diet: Focus on consuming lean protein sources such as chicken, fish, tofu, and legumes to support muscle maintenance and wound healing.
Hydration: Drink plenty of water throughout the day to stay hydrated and maintain optimal health. Avoid sugary beverages and excessive caffeine intake.
Vitamin and Mineral Supplementation: Start taking recommended supplements such as a multivitamin, calcium, vitamin D, and iron to prevent nutrient deficiencies post-surgery.
Low-Carb, Low-Sugar Diet: Limit your intake of high-carbohydrate and high-sugar foods to help shrink the liver and reduce the risk of complications during surgery.
Portion Control: Practice portion control and mindful eating habits to prepare for the smaller meals you’ll consume post-surgery.
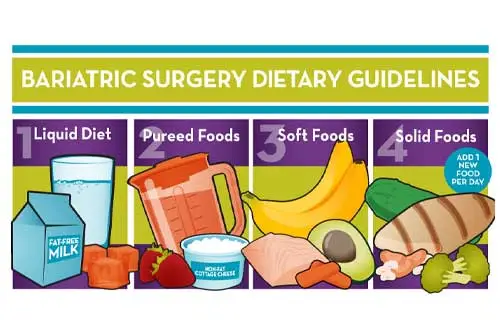
Post-Surgery Dietary Progression
After undergoing gastric bypass surgery, your stomach undergoes significant changes, requiring a carefully planned dietary progression to support healing, adjust to the new stomach size, and promote long-term weight loss success. Let’s explore each stage of the post-surgery dietary progression in detail:
Stage 1: Clear Liquid Diet (Days 1-7)
Allowed Foods:
Clear liquids such as water, broth, sugar-free gelatin, and herbal tea.
Purpose:
Prevent dehydration and promote healing.
Ease the transition from fasting to a liquid diet.
During this initial stage, clear liquids provide essential hydration and electrolytes while allowing the stomach to rest and heal from the surgical procedure. These easily digestible fluids help prevent dehydration, which is crucial for recovery. The simplicity of clear liquids also minimizes stress on the digestive system, allowing it to gradually adjust to the changes.
Stage 2: Full Liquid Diet (Weeks 2-3)
Allowed Foods:
Protein shakes, low-fat yogurt, skim milk, and strained soups.
Purpose:
Provide additional nutrients while still allowing the stomach to heal and adjust.
In the second stage, the diet progresses to include full liquids, which offer more nutritional variety and support optimal healing. Protein shakes become a primary source of nutrients, helping to maintain muscle mass and support the body’s recovery process. Low-fat yogurt and skim milk provide calcium and other essential nutrients, while strained soups offer nourishment in an easily digestible form.
Stage 3: Pureed Diet (Weeks 4-5)
Allowed Foods:
Pureed meats, soft-cooked vegetables, and mashed fruits.
Purpose:
Introduce more texture and variety while ensuring foods are easy to digest.
As the healing process continues, the diet advances to include pureed foods, which offer a greater variety of textures and flavors. Pureed meats provide essential protein, while soft-cooked vegetables and mashed fruits offer vitamins, minerals, and dietary fiber. These foods are blended to a smooth consistency, making them easier to swallow and digest as the stomach adjusts to its reduced size.
Stage 4: Soft Foods Diet (Weeks 6-8)
Allowed Foods:
Soft, easy-to-chew foods such as ground meats, cooked vegetables, and soft fruits.
Purpose:
Continue advancing the diet while avoiding foods that may cause discomfort or irritation.
In the soft foods stage, the diet expands to include foods that are soft and easy to chew, yet still provide essential nutrients. Ground meats offer protein without the need for extensive chewing, while cooked vegetables and soft fruits provide vitamins, minerals, and fiber. These foods are gentle on the digestive system, helping to prevent discomfort or irritation as the stomach continues to heal.
Stage 5: Regular Diet (Week 9 and Beyond)
Allowed Foods:
Gradually reintroduce solid foods, focusing on lean proteins, fruits, vegetables, and whole grains.
Purpose:
Establish long-term eating habits that support weight loss maintenance and overall health.
In the final stage of the dietary progression, solid foods are gradually reintroduced, allowing for a return to a more normal eating pattern. However, the emphasis remains on nutrient-dense, high-protein foods such as lean meats, fish, poultry, eggs, and plant-based proteins. Fruits, vegetables, and whole grains provide essential vitamins, minerals, and dietary fiber, supporting overall health and wellness. By establishing healthy eating habits early on, patients can maintain their weight loss and enjoy improved health and vitality in the long term.
Key Nutritional Considerations Post-Surgery
Protein Intake: Prioritize protein-rich foods to support healing, muscle maintenance, and satiety.
Hydration: Drink water throughout the day, but avoid drinking with meals to prevent overfilling the stomach.
Vitamin and Mineral Supplementation: Continue taking recommended supplements to prevent nutrient deficiencies.
Portion Control: Eat small, frequent meals and chew food thoroughly to prevent discomfort and ensure proper digestion.
Avoid Trigger Foods: Steer clear of high-sugar, high-fat, and carbonated beverages, as well as tough or dry meats and fibrous vegetables that may cause digestive issues.
Additional Tips for Success
Mindful Eating
Focus on Quality: Choose nutrient-dense foods that provide essential vitamins, minerals, and antioxidants to support overall health.
Listen to Your Body: Pay attention to hunger and fullness cues, and stop eating when you feel satisfied, rather than full.
Slow Down: Chew your food thoroughly and take your time with each meal to aid digestion and prevent discomfort.
Regular Physical Activity
Start Slow: Begin with low-impact activities such as walking, swimming, or cycling, and gradually increase intensity as you build strength and endurance.
Consistency is Key: Aim for at least 150 minutes of moderate-intensity exercise per week, spread out over several days, to support weight loss and improve cardiovascular health.
Incorporate Strength Training: Include resistance training exercises to build lean muscle mass, which can boost metabolism and aid in weight management.
Emotional Support
Seek Support: Join a support group or work with a therapist who specializes in weight management to address any emotional or psychological challenges related to food, body image, or lifestyle changes.
Practice Self-Compassion: Be kind to yourself and acknowledge that weight loss is a journey with ups and downs. Celebrate your successes and learn from setbacks without being too hard on yourself.
Regular Follow-Up Care
Stay Connected: Maintain regular follow-up appointments with your healthcare provider, surgeon, and dietitian to monitor your progress, address any concerns, and make adjustments to your diet and exercise plan as needed.
Be Proactive: Advocate for your health by asking questions, expressing any concerns or challenges you may be facing, and actively participating in your care plan.
Forbidden Foods After Gastric Bypass Surgery: What to Avoid for Optimal Health
Gastric bypass surgery is a transformative procedure that significantly reduces the size of the stomach and alters the digestive process. While this surgery can lead to substantial weight loss and improve overall health, it also requires patients to make significant dietary changes to support their new digestive system. Understanding which foods to avoid after gastric bypass surgery is essential to prevent complications, promote healing, and maintain long-term success. Here’s a comprehensive guide to forbidden foods after gastric bypass surgery:
1. High-Sugar Foods and Beverages:
Examples:
Sugary drinks (sodas, fruit juices, sweetened teas)
Desserts (cakes, cookies, pastries)
Candy and chocolates
Sweetened yogurt and ice cream
Reasons to Avoid:
High-sugar foods and beverages can lead to dumping syndrome, a condition characterized by rapid gastric emptying and symptoms such as nausea, vomiting, diarrhea, sweating, and dizziness.
These foods can also contribute to weight regain and increase the risk of developing metabolic conditions such as diabetes and insulin resistance.
2. High-Fat Foods:
Examples:
Fried foods (fried chicken, French fries, onion rings)
Fatty cuts of meat (bacon, sausage, ribs)
Processed meats (hot dogs, salami, sausage)
High-fat dairy products (whole milk, full-fat cheese, cream)
Reasons to Avoid:
High-fat foods are difficult to digest and may cause gastrointestinal discomfort, including bloating, gas, and diarrhea.
Consuming high-fat foods can also lead to weight regain and increase the risk of developing cardiovascular disease and other health issues.
3. Carbonated Beverages:
Examples:
Soda (cola, lemon-lime, root beer)
Sparkling water
Carbonated energy drinks
Reasons to Avoid:
Carbonated beverages can cause discomfort and bloating due to the gas they produce in the stomach.
The carbonation in these beverages can also stretch the stomach pouch and potentially lead to weight regain or other complications.
4. Tough or Dry Meats:
Examples:
Tough cuts of steak or roast beef
Dry chicken or turkey breast
Jerky or dried meats
Reasons to Avoid:
Tough or dry meats can be difficult to chew thoroughly and may cause discomfort or blockages in the digestive tract.
These foods can also be high in fat and protein, which may be challenging for the digestive system to handle in the early stages after surgery.
5. Fibrous or Stringy Vegetables:
Examples:
Raw carrots
Celery
Broccoli stalks
Asparagus
Reasons to Avoid:
Fibrous or stringy vegetables can be difficult to digest and may cause discomfort or blockages in the digestive tract.
While these vegetables are nutritious, it’s best to consume them cooked and well-cooked to make them easier to digest.
6. Sticky or Gummy Foods:
Examples:
Sticky candies (gummies, taffy)
Peanut butter
Rice cakes
Coconut flakes
Reasons to Avoid:
Sticky or gummy foods can adhere to the walls of the stomach pouch and cause discomfort or blockages.
These foods can also be high in sugar and calories, which may hinder weight loss efforts and increase the risk of complications.
7. Sugary Alcoholic Beverages:
Examples:
Sweetened cocktails (margaritas, daiquiris)
Liqueurs (Bailey’s Irish Cream, amaretto)
Sweet wines (dessert wines, sparkling wines)
Reasons to Avoid:
Sugary alcoholic beverages can contribute to dumping syndrome and may lead to rapid spikes in blood sugar levels.
These beverages are also high in empty calories and can hinder weight loss efforts, as well as increase the risk of alcohol-related complications after surgery.
8. Tough, Fibrous Fruits:
Examples:
Raw apples (with skin)
Pears (with skin)
Pineapple
Mango
Reasons to Avoid:
Tough, fibrous fruits can be difficult to digest and may cause discomfort or blockages in the digestive tract.
It’s best to consume these fruits in small amounts and well-cooked or blended into smoothies to make them easier to digest.
Conclusion
The journey before and after gastric bypass surgery involves careful attention to dietary choices to optimize outcomes and support long-term success. By following a structured diet plan that progresses gradually from clear liquids to solid foods, patients can ensure proper healing, minimize complications, and achieve sustainable weight loss. Additionally, maintaining a balanced diet rich in protein, vitamins, and minerals, while practicing portion control and mindful eating, is essential for maximizing the benefits of gastric bypass surgery and improving overall health and well-being. Always consult with a healthcare provider or a registered dietitian for personalized guidance and support throughout your weight loss journey.
Frequently Asked Questions (FAQs) About Diet After Gastric Bypass Surgery:
- What dietary changes are required after gastric bypass surgery?
Answer: After gastric bypass surgery, patients must transition to a modified diet to accommodate the reduced stomach size and altered digestive system. This typically involves progressing through several stages, starting with clear liquids and gradually advancing to pureed foods, soft foods, and eventually a regular solid diet.
- How soon after surgery can I start eating solid foods?
Answer: The timeline for reintroducing solid foods varies depending on individual healing and tolerance. Generally, patients can begin incorporating solid foods back into their diet about 6-8 weeks after surgery, following a gradual progression from liquids to pureed and soft foods.
- What types of foods should I focus on after gastric bypass surgery?
Answer: After gastric bypass surgery, it’s essential to prioritize nutrient-dense foods that are high in protein and low in fat and sugar. Lean meats, fish, poultry, eggs, dairy products, fruits, vegetables, and whole grains are excellent choices to support healing, promote weight loss, and ensure adequate nutrition.
- Are there any foods I should avoid indefinitely after gastric bypass surgery?
Answer: Yes, certain foods should be avoided or consumed sparingly after gastric bypass surgery to prevent complications and support long-term success. These include high-sugar foods and beverages, high-fat foods, carbonated beverages, tough or dry meats, fibrous vegetables, and sticky or gummy foods.
- How can I ensure I’m getting enough nutrients after gastric bypass surgery?
Answer: Meeting nutritional needs after gastric bypass surgery requires careful planning and monitoring. Patients are encouraged to focus on consuming protein-rich foods, taking prescribed vitamin and mineral supplements, staying hydrated, and practicing portion control. Regular follow-up appointments with healthcare providers and registered dietitians can also help ensure nutritional adequacy and address any concerns or deficiencies.