For the inaugural occasion, the NHS has administered water-filled gastric balloons to obese patients, marking a significant step in weight loss treatment.
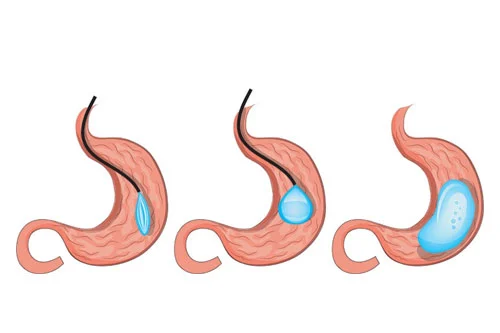
This innovative procedure involves ingesting a capsule containing a balloon that is subsequently filled with a pint of water. The filled balloon induces a feeling of fullness, encouraging patients to consume smaller portions of food. The entire process, lasting just 15 minutes, does not necessitate surgery, endoscopies, or sedation, resulting in reduced risk and cost.
Clinical studies have demonstrated that patients undergoing this treatment can shed up to 15% of their weight within four months. An automatic release valve opens the balloon after 16 weeks, facilitating the natural passage of both the water and the balloon from the body.
Musgrove Park Hospital in Somerset has treated two patients with this novel procedure on the NHS, marking the first instances of its application. Allurion, the manufacturer, received approval for NHS use in 2020 and has been engaging in discussions with hospital trusts to implement the treatment more widely.
The procedure, available privately at a cost ranging from £2,000 to £5,000, offers a more economical alternative to other weight loss interventions like gastric band surgery, gastric bypass, and sleeve gastrectomy, which often exceed £10,000.
Upcoming plans involve extending the treatment to three additional patients next month, with experts suggesting that millions of overweight and obese individuals could benefit from this approach.
Compared to other weight loss methods, such as the Wegovy injection costing around £3,000 for a year’s supply, the gastric balloon capsule is considered a cost-effective and less invasive option.
The procedure entails swallowing the capsule attached to a thin tube, with an x-ray confirming its placement before inflating the balloon with 550ml of water. A subsequent x-ray verifies the balloon’s position, and the tube is then removed.
While potential side effects include a sore throat, nausea, vomiting, reflux, and cramping, data indicates that patients were able to maintain 95% of their weight loss a year after the treatment. The procedure can be repeated, offering a flexible and promising solution for individuals grappling with severe obesity.
Professor Richard Welbourn, a consultant bariatric surgeon at Somerset NHS Foundation Trust, expressed satisfaction in providing this innovative treatment within a holistic weight loss program. Dr. Shantanu Gaur, the founder and CEO of Allurion, conveyed excitement about the partnership with the NHS, foreseeing the positive impact on many more patients in the future.