Weight loss surgery, also known as bariatric surgery, has become an increasingly popular option for individuals struggling with obesity and related health issues. These surgical procedures are designed to help patients lose weight by altering the digestive system’s anatomy, leading to reduced calorie intake and improved metabolic function. With several types of weight loss surgeries available, it’s essential to understand the differences between them to make informed decisions about treatment options. In this article, we’ll explore some of the most common types of weight loss surgery and their unique characteristics.
Gastric Bypass Surgery
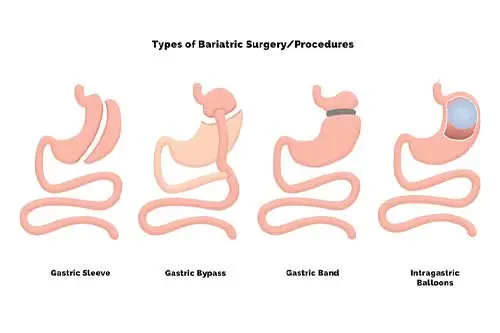
Gastric bypass surgery is one of the most commonly performed weight loss procedures. During this surgery, the surgeon creates a small pouch at the top of the stomach and connects it directly to the small intestine, bypassing a portion of the stomach and the upper part of the small intestine. This results in reduced food intake and decreased absorption of calories and nutrients. Gastric bypass surgery often leads to significant weight loss and improvement in obesity-related health conditions such as type 2 diabetes and high blood pressure.
with gastric bypass surgery, it’s essential to understand both the benefits and potential risks associated with this procedure.
Benefits
Significant Weight Loss: Gastric bypass surgery typically results in substantial weight loss, with patients often losing 60-80% of their excess body weight within the first year after surgery.
Improvement or Resolution of Health Conditions: In addition to weight loss, gastric bypass surgery can lead to the improvement or resolution of various obesity-related health conditions, including type 2 diabetes, high blood pressure, sleep apnea, and joint pain.
Long-term Results: Many patients experience long-term weight loss success following gastric bypass surgery, with sustained improvements in overall health and quality of life.
Enhanced Metabolic Health: The rerouting of the digestive tract in gastric bypass surgery can positively impact metabolic function, leading to better blood sugar control and insulin sensitivity.
Risks
Surgical Risks: As with any surgical procedure, gastric bypass surgery carries inherent risks, including infection, bleeding, blood clots, and adverse reactions to anesthesia.
Nutritional Deficiencies: Due to the alteration of the digestive tract, gastric bypass patients are at risk of developing nutritional deficiencies, particularly in vitamins and minerals such as vitamin B12, iron, calcium, and folate. Lifelong supplementation and regular monitoring are essential to prevent deficiencies.
Dumping Syndrome: Dumping syndrome is a common complication of gastric bypass surgery characterized by rapid gastric emptying, leading to symptoms such as nausea, vomiting, abdominal cramps, diarrhea, and lightheadedness after eating certain foods, especially those high in sugar or fat.
Gallstones: Rapid weight loss following gastric bypass surgery can increase the risk of developing gallstones, which may require additional treatment, including medication or surgery.
Lifestyle Changes: Successful long-term outcomes after gastric bypass surgery require significant lifestyle modifications, including adherence to a specific dietary regimen, regular physical activity, and lifelong medical follow-up.
Sleeve Gastrectomy
Sleeve gastrectomy, also known as gastric sleeve surgery, involves the removal of a large portion of the stomach, leaving behind a narrow tube or sleeve-shaped stomach. By reducing the stomach’s size, sleeve gastrectomy restricts the amount of food that can be consumed, leading to feelings of fullness and decreased appetite. Unlike gastric bypass surgery, sleeve gastrectomy does not involve rerouting the intestines. This procedure has gained popularity due to its effectiveness in promoting weight loss and its relatively low risk of complications.
Sleeve gastrectomy, also referred to as gastric sleeve surgery, has emerged as a popular and effective weight loss procedure in recent years. Unlike some other bariatric surgeries, such as gastric bypass, sleeve gastrectomy does not involve rerouting the intestines. Instead, it focuses on reducing the size of the stomach to limit food intake and promote weight loss.
During sleeve gastrectomy surgery, a large portion of the stomach is surgically removed, leaving behind a narrow tube or sleeve-shaped stomach. This smaller stomach size significantly restricts the amount of food that can be consumed, leading to feelings of fullness and decreased appetite. Additionally, the surgery removes the part of the stomach that produces the hunger hormone ghrelin, further reducing food cravings.
One of the key benefits of sleeve gastrectomy is its effectiveness in promoting significant and sustainable weight loss. Many patients experience substantial weight loss in the months following surgery, with continued progress over the following years. This weight loss not only improves physical health but also enhances overall quality of life and self-esteem.
In addition to weight loss, sleeve gastrectomy often leads to improvement or resolution of obesity-related health conditions, such as type 2 diabetes, high blood pressure, and sleep apnea. By achieving better control over these conditions, patients can reduce their reliance on medications and lower their risk of developing complications associated with obesity.
The recovery process after sleeve gastrectomy typically involves a hospital stay of 1-2 days, during which patients are closely monitored for any post-operative complications. Most individuals can return to normal activities within 2-4 weeks but may need to follow a specific diet plan recommended by their healthcare provider to ensure proper healing and maximize weight loss results.
While sleeve gastrectomy is generally considered safe, it is essential to be aware of the potential risks and complications associated with any surgical procedure. These may include infection, bleeding, blood clots, leakage at the staple line, gastrointestinal issues such as acid reflux or nausea, and vitamin and mineral deficiencies. However, the likelihood of experiencing complications is relatively low, especially when the surgery is performed by an experienced bariatric surgeon and comprehensive pre-operative evaluation and post-operative care are provided.
Adjustable Gastric Banding
Adjustable gastric banding, commonly referred to as lap band surgery, involves placing an inflatable silicone band around the upper part of the stomach to create a smaller stomach pouch. The band can be adjusted by adding or removing saline solution through a port placed under the skin. This adjustment allows for control over the size of the stomach opening and the rate of weight loss. Adjustable gastric banding is considered less invasive than other weight loss surgeries and is reversible, making it an attractive option for some patients.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
Biliopancreatic diversion with duodenal switch is a complex weight loss procedure that involves two steps. The first step is similar to a sleeve gastrectomy, where a portion of the stomach is removed to create a smaller stomach pouch. In the second step, a significant portion of the small intestine is bypassed, rerouting the digestive tract to limit calorie absorption further. BPD/DS results in significant weight loss and may be recommended for individuals with severe obesity or obesity-related health conditions.
However, due to its complexity and potential for nutritional deficiencies, Biliopancreatic Diversion with Duodenal Switch (BPD/DS) is typically reserved for individuals with severe obesity or those who have not achieved successful weight loss with other surgical interventions.
The first step of the procedure involves the removal of approximately 70-80% of the stomach, leaving behind a smaller, tube-shaped stomach or pouch. This restrictive component limits the amount of food that can be consumed, leading to feelings of fullness with smaller meals.
In the second step, a significant portion of the small intestine is rerouted to bypass the duodenum and part of the jejunum. This bypass reduces the absorption of calories and nutrients, further contributing to weight loss. However, it also diminishes the body’s ability to absorb essential vitamins and minerals, increasing the risk of nutritional deficiencies.
Despite its effectiveness in achieving substantial weight loss, BPD/DS requires lifelong monitoring and adherence to strict dietary and supplement regimens to prevent complications. Patients must work closely with a multidisciplinary healthcare team, including dietitians, surgeons, and endocrinologists, to optimize outcomes and minimize risks.
While Biliopancreatic Diversion with Duodenal Switch may offer significant benefits for individuals with severe obesity, it is not without potential drawbacks. Complications associated with the procedure can include malnutrition, dumping syndrome, gastrointestinal issues, and long-term vitamin deficiencies. Therefore, careful consideration and thorough evaluation by healthcare professionals are essential before undergoing this type of weight loss surgery.
Intragastric Balloon
Intragastric balloon placement is a non-surgical weight loss procedure that involves inserting a deflated balloon into the stomach and then inflating it with saline solution. The balloon takes up space in the stomach, leading to feelings of fullness and reduced food intake. Intragastric balloons are typically left in place for a limited period, usually six months, after which they are removed. This procedure may be suitable for individuals who are not candidates for or prefer to avoid surgery.
Allurion Gastric Balloon
The Allurion Gastric Balloon is a specific type of intragastric balloon designed to aid in weight loss for individuals seeking a non-surgical approach. This innovative device offers a minimally invasive option for those who may not qualify for or prefer to avoid traditional weight loss surgeries.
The Allurion Gastric Balloon works on the principle of gastric restriction, similar to other intragastric balloons. It consists of a soft, silicone balloon that is inserted into the stomach in its deflated state. Once in place, the balloon is filled with a saline solution, expanding to occupy space within the stomach.
By occupying space in the stomach, the balloon creates a feeling of fullness and satiety, helping individuals consume smaller portions of food and reduce overall calorie intake. This reduction in food consumption can lead to gradual and sustainable weight loss over time.
One of the key advantages of the Allurion Gastric Balloon is its innovative delivery system, which allows for a straightforward and outpatient procedure. Unlike traditional intragastric balloons that require endoscopic insertion, the Allurion balloon is swallowed in a capsule form and then inflated with a thin catheter. This process eliminates the need for anesthesia and reduces the risk of complications associated with traditional balloon placement methods.
Additionally, the Allurion Gastric Balloon is designed to be temporary, typically remaining in the stomach for approximately six months. At the end of the treatment period, the balloon is safely deflated and removed during a brief outpatient procedure, allowing patients to return to their normal activities quickly.
The Allurion program also includes comprehensive support and guidance to help patients maximize their weight loss results. This may include nutritional counseling, lifestyle modifications, and behavior therapy to promote healthy habits and long-term success.
While the Allurion Gastric Balloon offers a promising option for individuals seeking a non-surgical approach to weight loss, it is essential to consult with a healthcare provider to determine if it is the right choice for you. As with any medical procedure, there are potential risks and benefits to consider, and a thorough evaluation by a qualified healthcare professional can help ensure safe and effective treatment outcomes.
Conclusion
Weight loss surgery offers a range of options for individuals seeking to achieve significant and sustained weight loss. Each type of weight loss surgery has its unique benefits, risks, and considerations, making it essential for patients to consult with healthcare providers to determine the most appropriate treatment plan. While weight loss surgery can be highly effective, it is not a cure-all and requires commitment to lifestyle changes, including dietary modifications and regular exercise, to achieve long-term success. By understanding the different types of weight loss surgery and their potential outcomes, patients can make informed decisions about their health and well-being.
FAQs
What are the different types of weight loss surgery available?
Answer: There are several types of weight loss surgery, including gastric bypass, sleeve gastrectomy, adjustable gastric banding (lap band), biliopancreatic diversion with duodenal switch (BPD/DS), and intragastric balloon placement.
How do I know which weight loss surgery is right for me?
Answer: The best weight loss surgery for you depends on various factors, including your overall health, BMI (body mass index), obesity-related health conditions, and personal preferences. It’s essential to consult with a healthcare provider who specializes in bariatric surgery to determine the most suitable option based on your individual needs.
What are the risks and benefits associated with each type of weight loss surgery?
Answer: Each weight loss surgery procedure has its own set of risks and benefits. Generally, benefits include significant weight loss, improvement or resolution of obesity-related health conditions, and enhanced quality of life. Risks may include complications such as infection, bleeding, leakage, nutritional deficiencies, and gastrointestinal issues. Your healthcare provider can provide detailed information about the risks and benefits of each procedure.
How long does it take to recover from weight loss surgery?
Answer: Recovery time varies depending on the type of weight loss surgery performed and individual factors such as overall health and surgical approach. In general, patients can expect to stay in the hospital for a few days after surgery and may need several weeks to months to fully recover. Your healthcare team will provide specific instructions for post-operative care and follow-up appointments.
Will I need to make lifestyle changes after weight loss surgery?
Answer: Yes, weight loss surgery is a tool to help you lose weight, but long-term success requires commitment to lifestyle changes. This typically includes adopting a healthy diet, incorporating regular physical activity, attending follow-up appointments, and addressing any emotional or psychological factors related to weight management. Your healthcare team will provide support and guidance throughout your weight loss journey.